Introduction to lactose intolerance
Lactose intolerance is a common digestive disorder. It occurs when the body doesn't produce enough of the enzyme lactase. This enzyme is necessary to break down milk sugar (lactose). If the body can't digest lactose properly, it passes unchanged into the large intestine. This leads to unpleasant symptoms such as bloating, abdominal pain, and diarrhea. The intolerance can be genetic or develop over time. One reason for this could be a decrease in lactase production in adulthood.
This text is aimed at people who are personally affected by lactose intolerance. It also appeals to those who are interested in the topic for personal or professional reasons. Raising awareness about the symptoms and effects of lactose intolerance is important. It helps those affected adjust their diet and improve their quality of life. Furthermore, understanding this digestive disorder helps eliminate misconceptions and prejudices, making it easier to create a supportive environment for those affected.
Biological background of lactose intolerance
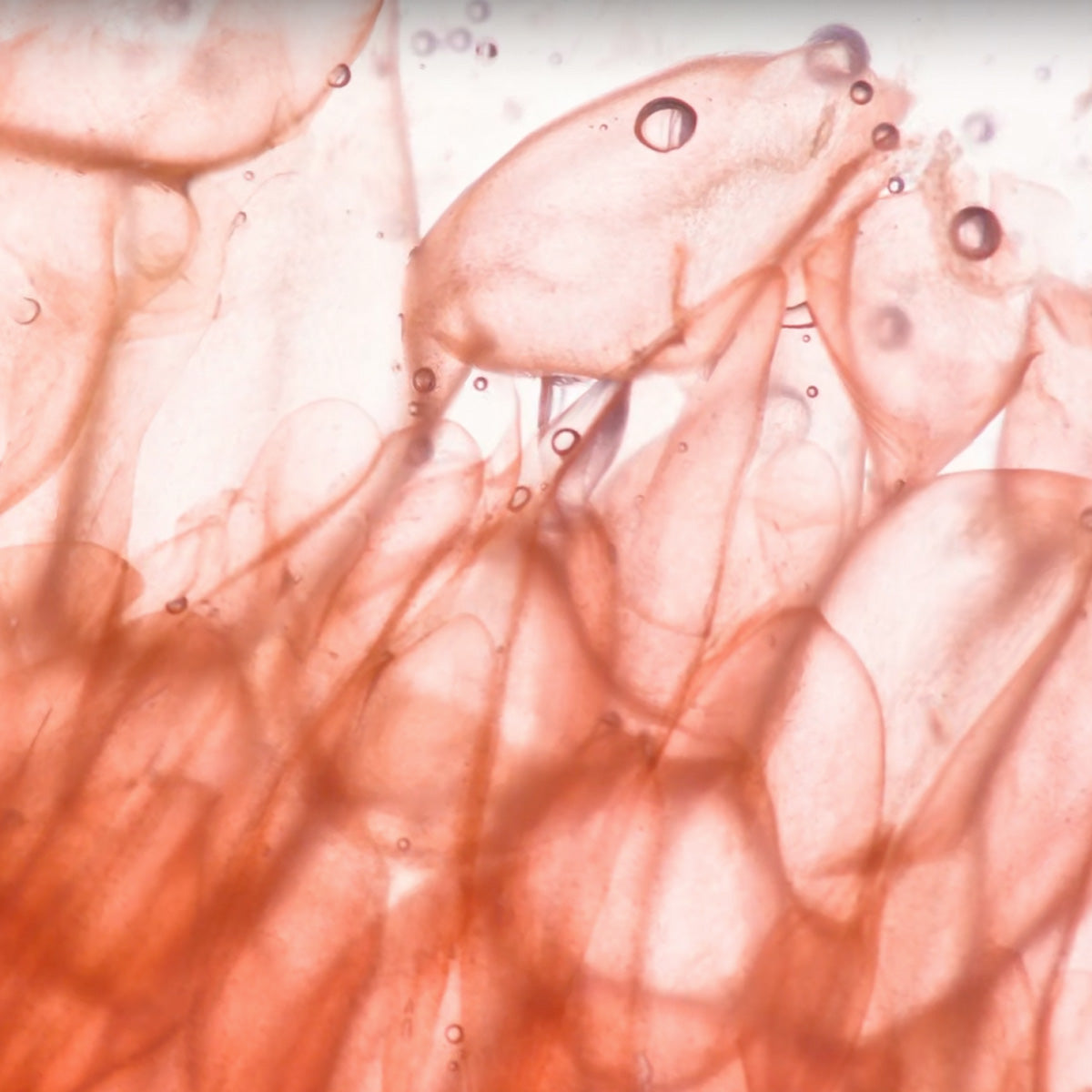
The digestion of lactose, the sugar in dairy products, is a complex process that takes place in the digestive tract. Lactose first passes through the stomach into the small intestine. There, it is broken down by the enzyme lactase, produced in the villi lining the small intestine wall. This breakdown process converts lactose into its components, glucose and galactose, which are then easily absorbed by the body. These glucose and galactose then enter the bloodstream to serve as an energy source for the body (1).
The enzyme lactase plays a crucial role in lactose processing. Lactase production is influenced by genetic predisposition and varies from person to person. People who produce sufficient lactase digest lactose without problems and do not experience any discomfort after consuming dairy products (2).
Primary lactose intolerance occurs when lactase production naturally decreases over time, especially after childhood. This occurs in many people worldwide and explains why many adults have difficulty digesting dairy products. Most affected individuals suffer from this form of the condition.
There is also what is known as secondary lactose intolerance. This is an intolerance resulting from a small intestinal disease. This disease impairs the production of lactase. Causes can be an infection or surgery. In both cases, a lactase deficiency leads to poor digestion of lactose and results in the typical symptoms of lactose intolerance (3).

Symptoms of lactose intolerance
Lactose intolerance causes a variety of symptoms that manifest in different ways and impair the quality of life of those affected. The most common symptoms that occur immediately after consuming lactose-containing foods are abdominal pain, bloating, and diarrhea. These symptoms usually occur when consuming dairy products or other lactose-containing foods and last between 30 minutes and two hours after consumption. They are caused by the incomplete digestion of lactose. The undigested lactose then reaches the large intestine and is fermented by intestinal bacteria. This leads to gas, abdominal pain, and diarrhea (4,5).
In addition to the obvious gastrointestinal symptoms, less obvious signs can also indicate lactose intolerance. These include fatigue, headaches, concentration problems, skin problems such as eczema or itching, and mood swings, including depression. These symptoms can severely impair quality of life and negatively impact daily well-being. This is true even if they are not directly related to digestive problems (6).
Early diagnosis is important for initiating appropriate treatment and necessary lifestyle changes early. In the case of lactose intolerance, timely identification allows those affected to adjust their diet. They can avoid foods containing lactose. This helps reduce symptoms and improve quality of life. It is important for everyone to closely monitor their symptoms. If necessary, a doctor should be consulted. This will ensure a sound diagnosis and appropriate treatment. (7,8)
Diagnosis of lactose intolerance
Diagnosing lactose intolerance requires a careful examination of symptoms. Various tests are available to provide an accurate assessment. There are several procedures for diagnosing lactose intolerance. One of the most common tests is the hydrogen breath test. In this test, the individual drinks a solution containing lactose. The hydrogen level in the breath is then measured regularly over several hours. An increase in the hydrogen level indicates that the lactose is not being fully digested and is instead being fermented in the large intestine.
Another test is the stool test, which examines stool for the presence of undigested lactose. This test is often used in infants and young children because it is particularly straightforward (9).
A medical consultation plays a crucial role in diagnosing lactose intolerance. A doctor can assess the patient's symptoms, consider the medical history, and perform or recommend appropriate diagnostic tests. They can also order further tests, if necessary, to rule out other causes of the symptoms.
Collaboration with nutrition experts can also be beneficial. These include nutritionists or dietitians. They support patients in adjusting their diet. These professionals help develop an individualized diet plan. This plan restricts or replaces foods containing lactose. This can alleviate symptoms and ensure a balanced diet. (10,11)
It's important to clarify potential misconceptions and myths surrounding the diagnosis of lactose intolerance. A common misconception is that lactose intolerance only occurs in people of Asian or African descent. This is not the case. The condition can affect people of all ethnic groups. It should also be noted that lactose intolerance is not the same as a milk allergy. These two conditions are different and require different diagnostic and treatment approaches. While lactose intolerance is caused by an inability to tolerate the milk sugar, a milk allergy is caused by the immune system reacting to the proteins.

Lactose-free diet: Practical tips for everyday life with lactose intolerance
For people with lactose intolerance, a lactose-free diet is often essential to avoid symptoms. It's important to be aware of which foods contain lactose and should be avoided. These include milk and dairy products such as yogurt, cheese, cream, and butter. Convenience foods and foods with hidden lactose, such as sausages, baked goods, sauces, and dressings, should also be avoided.
Fortunately, there are a variety of alternative lactose-free products specifically made for people with lactose intolerance. These include lactose-free milk and dairy products, as well as plant-based milk alternatives such as almond, soy, oat, or rice milk. Natural yogurt with no added sugar or probiotic plant-based yogurt alternatives are also good alternatives: Many people with only mild intolerance can still consume yogurt. The reason appears to be the fermentation process using lactic acid bacteria (12,13).
When shopping, it's important to carefully read nutrition labels on food packaging to identify hidden lactose. Fresh, unprocessed foods such as fruits, vegetables, whole grains, meat, and fish are naturally lactose-free and therefore a safe choice. Supermarkets and pharmacies also carry specially labeled lactose-free products to help you choose.
When preparing meals at home, it's advisable to avoid ingredients containing lactose. When dining at a restaurant, it's helpful to check the menu in advance and ask about lactose-free options. You can also request special preparations without milk or cream, as well as lactose-free alternatives, at the restaurant.
It can also be helpful to keep lactose-free snacks and meals on hand. This ensures you always have an option at hand. Experimenting with lactose-free recipes can help you discover new flavors, opening up entirely new culinary possibilities. It's also important to be open about your lactose intolerance. Ask family, friends, and colleagues for their support and understanding.
Lactose intolerance in children and the elderly
Lactose intolerance can occur in both children and older adults and presents a particular challenge at both stages of life. A diagnosis of lactose intolerance in children can be alarming. Children often enjoy consuming dairy products. These products are an important part of a balanced diet. Parents must therefore pay particular attention to ensuring their children receive certain nutrients such as calcium and vitamin D. Most children consume these nutrients through milk and may be deficient.
Transitioning children to a lactose-free diet requires careful planning and creative solutions. Parents can use lactose-free dairy products. They can ensure their children receive a balanced diet that includes alternative sources of calcium, such as green vegetables, almonds, and fortified plant-based milk alternatives. (14)
Diagnosing lactose intolerance can also be challenging for older people, especially if they already suffer from other health problems. Restricted dietary intake can further complicate the situation. Digestion is often less efficient in old age, which can worsen the symptoms of lactose intolerance. Therefore, careful selection of lactose-free foods and adequate nutrient intake are especially important (15).
Patience is important when managing lactose intolerance in children and the elderly. A supportive environment helps manage symptoms. Parents can support their children by involving them in food shopping and preparation. They should also offer age-appropriate lactose-free recipes and snack ideas. With older adults, their individual needs and preferences must be considered. It is important to provide them with a diet that they enjoy and supports their health.
Conclusion and outlook
Overall, lactose intolerance is a widespread problem that affects many people, regardless of age. Proper diet and management of this condition are crucial to controlling symptoms.
With proper diagnosis and a customized diet, people with lactose intolerance can effectively control their symptoms. It's important to switch to lactose-free foods and find alternative sources of calcium to ensure a balanced diet.
It's also helpful to build a supportive community and engage with other sufferers. By sharing experiences and tips, people with lactose intolerance can learn from and encourage each other.
Further research and developments will continue to advance our understanding of lactose intolerance. It remains important to stay informed about the latest findings. By taking active steps and regularly staying informed, you can ensure you are in control of your health and well-being.
Sources
- Forsgård RA. Lactose digestion in humans: intestinal lactase appears to be constitutive whereas the colonic microbiome is adaptable. At J Clin Nutr. 2019 Aug 1;110(2):273-279. doi: 10.1093/ajcn/nqz104. PMID: 31175813; PMCID: PMC6669050.
- Lactase Capsules & Tablets: Uses & Side Effects (clevelandclinic.org) (March 17, 2024)
- Lactose Intolerance: Background, Pathophysiology, Etiology (medscape.com) (March 17, 2024)
- Lactose Intolerance | Johns Hopkins Medicine (March 17, 2024)
- Lactose intolerance - Symptoms & causes - Mayo Clinic (17.3.2024)
- https://www.healthline.com/nutrition/lactose-intolerance-symptoms (3/18/2024)
- Lactose intolerance - Diagnosis & treatment - Mayo Clinic (18.3.2024)
- Mattar R, de Campos Mazo DF, Carrilho FJ. Lactose intolerance: diagnosis, genetic, and clinical factors. Clin Exp Gastroenterol. 2012;5:113-21. doi: 10.2147/CEG.S32368. Epub 2012 Jul 5. PMID: 22826639; PMCID: PMC3401057.
- Diagnosis of Lactose Intolerance - NIDDK (nih.gov) (18.3.2024)
- Eating, Diet, & Nutrition for Lactose Intolerance - NIDDK (nih.gov) (18.3.2024)
- Treatment for Lactose Intolerance - NIDDK (nih.gov) (18.3.2024)
- Lactose-Free Diet: Foods to Eat and Avoid (healthline.com) (March 18, 2024)
- 5 Foods High in Lactose to Avoid (webmd.com) (3/20/2024)
- Lactose Intolerance in Children (nationwidechildrens.org) (March 20, 2024)
- Di Stefano M, Veneto G, Malservisi S, Strocchi A, Corazza GR. Lactose malabsorption and intolerance in the elderly. Scand J Gastroenterol. 2001 Dec;36(12):1274-8. doi: 10.1080/003655201317097119. PMID: 11761016.




















Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.